The purpose of this series on Supraventricular Tachyarrhythmias is to share what I’ve learned so far in my study, in the hopes that it may help someone else, perhaps in getting up to speed on the topic. Quick disclaimer: I’m still a beginner to the world of cardiology and electrophysiologic testing, so this may contain errors. Unless otherwise cited, the content of this series comes from a book entitled “Fogoros’ Electrophysiologic Testing”, by Dr. Richard N. Fogoros and John M. Mandrola.
Supraventricular Tachyarrhythmias are a group of arrhythmias that are non-lethal, and that occur above the ventricles, usually in the atria. They have the effect of increasing the heart rate. These tachycardia can be broadly divided into two classes, automatic and reentrant. We’ll talk about each one in turn, and the underlying mechanisms that make them possible.
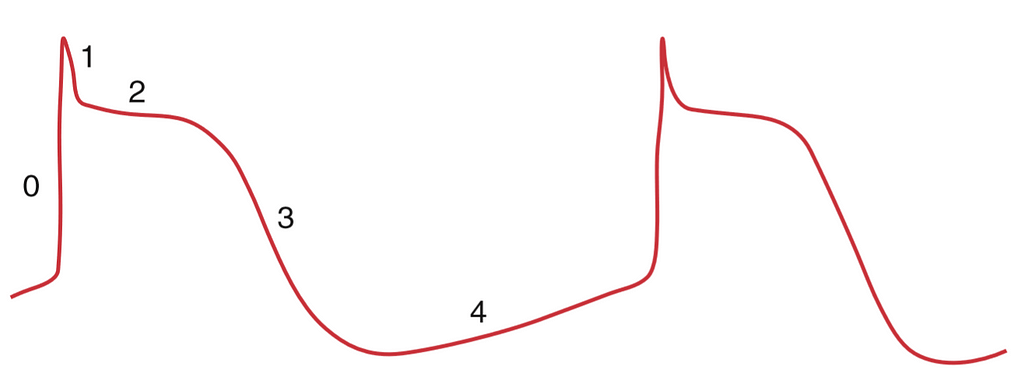
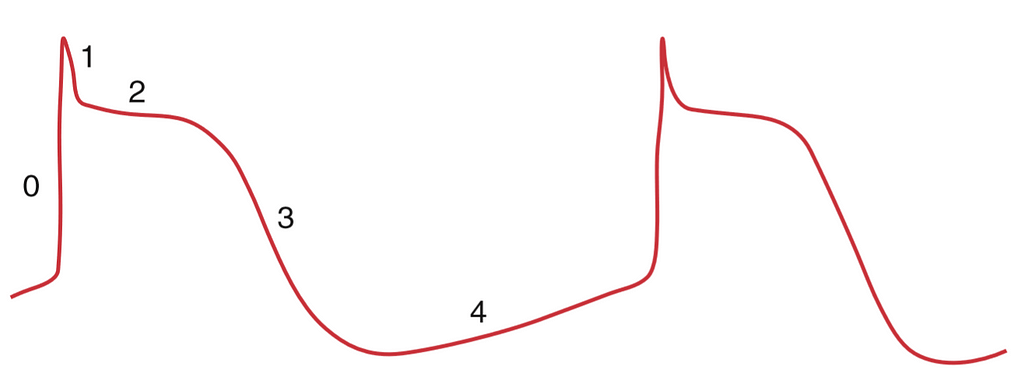
This class of tachyarrhythmias are made possible by misbehaving automaticity within the heart. Automaticity is a phenomenon where a cardiac cell, or more commonly, a group of them, has a leaky cell membrane, that triggers another action potential, “automatically”. This is represented in stage 4 of the figure. This phenomenon, when functioning normally, is what powers your heart’s pacemaker cells, and makes sure your heart continues to beat.
Automatic Atrial Tachycardia (AAT) is caused by an additional pacemaker node, or automatic focus, in the atrial muscle wall, or myocardium. This additional automatic focus causes tachycardia, where its pacing is faster than that of the SA node.
Multifocal Atrial Tachycardia (MAT) is much the same, except there are more automatic foci in the atrium. Each of the automatic foci fire independently, and this results in tachycardia. In MAT, the p-waves observed in a surface ECG look different, like in the image shown below.

This is a condition where the heart beats faster than normal, but for no apparent reason. The condition presents identically to Normal Sinus Tachycardia, with a major distinction being that there is no apparent reason for the tachycardia. Resting heart rates may be around 100bpm, and they increase even more on exertion. We are not sure what the cause of IST is, but it seems to frequently occur after a viral infection or physical trauma. It also appears to occur commonly in women in their 20s and 30s.

The mechanism of Reentrant Supraventricular Tachyarrhythmias is a reentrant circuit. Reentrant circuits, in the cardiac context, are circuits where a signal conducted across two different pathways may reenter the conduction pathway, resulting in a self-perpetuating cycle of signal conduction.
A core assumption here is that pathway A conducts slower, and has a shorter refractory period. Pathway B conducts faster, but has a longer refractory period. A signal that originates at the top of the diagram may conduct through both pathways. The signal conducted through A may reach conduct into B, which then continues conducting all the way through A again, creating a perpetual loop.
In AVNRT, there are dual conducting pathways in the AV Node. The entire reentrant circuit exists in the AV Node.
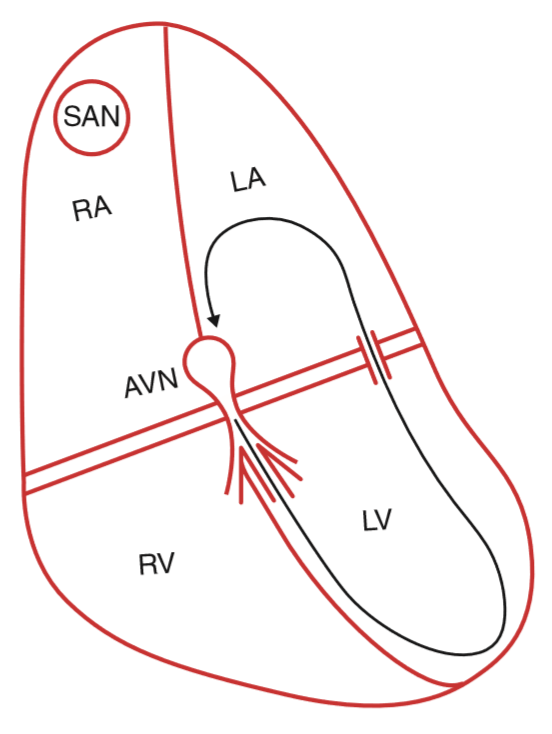
In Bypass Tract-Mediated Macroreentrant Tachycardia, the reentrant circuit goes through multiple regions of the heart, hence the macro prefix, and involves a bypass tract portion. This bypass portion could be created by a hereditary condition, like Wolff-Parkinson-White syndrome, or another bypass tract. These other bypass tracts are usually only functional in one direction, the retrograde direction.
Intraatrial reentry occurs when the reentrant circuit is completely within the atria, and does not include the AV node at all. This type of reentrant circuit generates P waves that look different from the standard sinus P wave.
Like the name implies, this reentry circuit is contained within the SA Node. This type of reentry is interesting in that it is spontaneously occurring, and Atrial Fibrillationdoes not exhibit the warm-up behavior that is usually observed with normal sinus tachycardia. The P waves it produces are identical to normal sinus P waves.
Atrial flutter involves a reentrant circuit in the atria of the heart. It is kicked off by a premature atrial impulse, which “jumpstarts” the reentrant circuit. Atrial Flutter is often observed with 2:1 AV block, which means that 2 P waves are observed for every QRS complex. Atrial flutter can result in heart rates at or over 220 bpm.
Atrial Fibrillation, or AFib, is a condition where atrial and ventricular activity is chaotic and uncoordinated. In the image below is an example of AFib where a P wave is not observable.

<hr><p>Supraventricular Tachyarrhythmias: An Overview was originally published in Medical CPS on Medium, where people are continuing the conversation by highlighting and responding to this story.</p>